Competing with the giants of the industry is more than possible with the right approach, and there are three pivotal ways private physician practices can fight back against extinction and ensure longevity.
APRIL 2024

As healthcare has evolved over time, so has the prevalence of private physician practices. What was once a common occurrence for patients—heading to the family-owned doctor’s office—has in many cases been replaced by the experience of seeking care at a network of physicians employed by large organizations.
Cumulative Number of Private Equity Acquisition Deals of Physician Practices by Specialty, 2012-2021
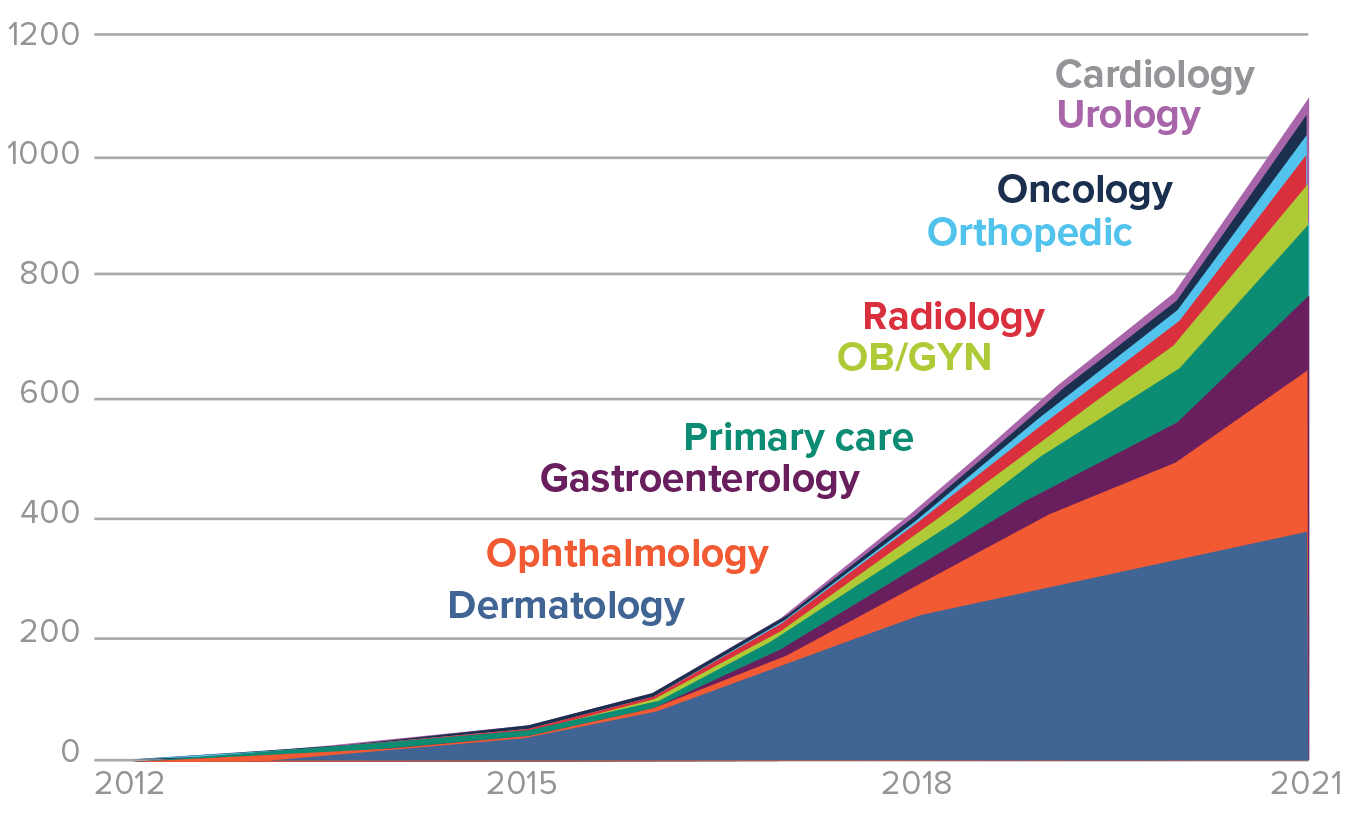
SOURCE: Authors’ analysis of PitchBook Data, Inc., as of June 15, 2022. PitchBook data has not been reviewed by PitchBook analysts.
How Did We Get Here?
“You can attribute that mainly to two things,” David Eagle, vice president of the American Independent Medical Practice Association and chair of Legislative Affairs and Patient Advocacy at New York Cancer & Blood Specialists, tells HealthLeaders. “There's just been a difference in the playing field between us and our competitors in terms of reimbursement and support for the practice model. So that's been the driving force over the last 40 years producing that.”
It’s becoming harder and harder for practices to maintain their independence, but it’s far from impossible. What it does require is physicians understanding where they want to fall on the “liberty versus security” spectrum, Ron Holder, COO at Medical Group Management Association (MGMA) tells HealthLeaders. Operating independently can be liberating and fulfilling in many ways, but an all-encompassing approach to providing care comes with heavy responsibility, particularly on the business side of things.
The Drop in Private Practice
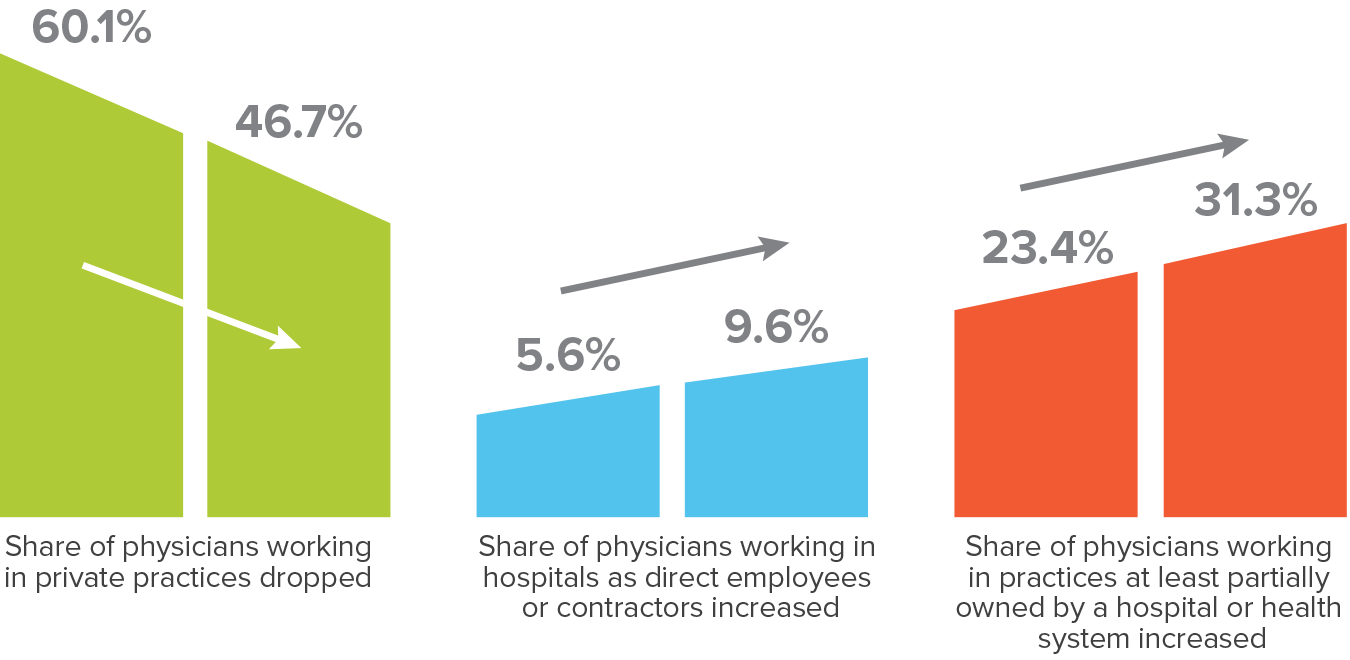
SOURCE: American Medical Association (AMA).
“The very first thing you need to understand is what’s not working. Do you as a physician—an independent physician or as the leader of the practice—have the capacity to manage and make tough decisions?”
—Ron Holder, COO at Medical Group Management Association
Knowing when to partner
That’s why the first step to making sure you can keep an independent practice is to have the right people with the ability to steer the practice.
“The very first thing you need to understand is what’s not working,” Holder says. “Do you as a physician, as an independent physician or as the leader of the practice, have the capacity to manage and make tough decisions?”
“The practice either has to have a physician who is a true expert at practice administration or they're going to need to partner with a management service organization (MSO) that can help provide that expertise,” Eagle says. “That's fundamental.”
One of the most important decisions physician practices must make is determining what they need to own and run themselves versus what they want to contract or bring on a partner for.
MSOs are one example of that. By joining these organizations, practices can hand off business functions like billing, compliance, information technology, and accounting, while still having autonomy over clinical decision-making.
The private equity-backed MSO model for independent physician practices has grown in presence over the past half decade and in addition to the access it provides to business talent, these organizations allow practices to tap into something necessary for survival: capital. Whether it’s to open new clinics or improve the quality of an existing office, having that type of financial backing can make all the difference in a practice thriving or dying out.
Joining an MSO or an independent practice association (IPA) does come with the understanding that physicians are surrendering some control over certain parts of the practice and you have to make financially optimal decisions at times, but it doesn’t mean selling your soul.
“One of the things that a lot of physicians don't understand is being independent doesn't mean that you have to own everything,” Holder says. “You can be an independent practice and still outsource or join with other physicians in a practice association, and share resources, purchasing agreements, human resources support, management services revenue, billings and collection, and still have some independence with regards to your own practice.”
Yet physicians want to serve their patients. Being a business owner may have appeal, but having the ability to shape how care is delivered is the biggest benefit for many physicians opting to run a private practice.
To truly put the focus on patients, physicians can absolve themselves of much of the administrative burden that any practice will encounter by bringing in partners to handle the less desirable functions of a practice.

Ron Holder
COO
Medical Group Management Association (MGMA)
Revenue cycle management is chief among those functions and more specifically, prior authorization is an area physicians can greatly benefit from outsourcing.
“I can tell you in my current experience in New York, prior authorization is just a terrible problem,” Eagle says. “It's time consuming, it results in meaningful treatment delays for patients, and frankly it's just random.”
According to a survey of over 1,000 physicians by the AMA, 88% of respondents said the burdens associated with prior authorization are high or extremely high. Physicians also revealed that practices complete 45 prior authorizations per physician per week, which equates to nearly two business days (14 hours).
Utilizing outside parties to take that and other kinds of responsibility off your plate can free up physicians for more meaningful work.
46%
Percentage of physicians
working in private practices as of 2022, according to the AMA.
Solve for Reimbursement
The main challenge that is driving practices to merge with health systems and other organizations is one that isn’t going away anytime soon.
Reimbursement remains a Rubik’s Cube for smaller providers operating at a disadvantage in terms of negotiating power. Joining an MSO or IPA can also allow practices to negotiate higher reimbursement rates, but those partnerships aren’t the only way for physicians to improve their ability to negotiate while staying independent.
First and foremost, practices should learn what the prevailing reimbursement rates are to avoid being taken advantage of by payers. Hiring a consultant or an attorney to come in and inform you about the value of your specialty on the market, as well as negotiate on your behalf, can be valuable.
Once you are aware of what the rates are, you can work on improving your position. Be aware that this takes a commitment to building relationships to get referrals, especially if you are just coming into the market. For those providing tertiary or quaternary care, building a referral network takes significant time and energy, but is critical to creating a pipeline and ensuring your practice can sustain itself. It’s not just about the quantity of referrals either, but the quality of them. Securing referrals for patients with insurance needs to be the goal.
“Just like in any negotiation, you want to be coming from a position of strength,” Holder says. “If you go into a car dealership and everybody involved from the minute you walk in the door knows that you need a car and knows that you're going to buy that car, guess what? You have no position of strength. It's been completely eroded. So if you're someone that has established that you are a great physician to work with as a referrer or referee and you've got good clinical outcomes, you're that unicorn. That makes you attractive to the payers.”
David Eagle
Vice President of the American Independent Medical Practice Association and chair of Legislative Affairs and Patient Advocacy
New York Cancer & Blood Specialists
“There's a difference in the playing field between us and our competitors in terms of reimbursement and support for the practice model.”
—David Eagle, vice president of the American Independent Medical Practice Association, says about why the number of private physician practices are dwindling.
The payer-provider dynamic doesn’t only have to be adversarial because of negotiations on fee-for-service payments. Pursuing a value-based care model can be beneficial for everyone involved, including patients, and allow practices to mitigate their costs.
However, a value-based approach requires that providers are willing to take on and manage risk. This can be especially difficult for newer practices. For established practices, it’s an avenue to explore if you have a track record of providing services to your patients at less than what you’re being reimbursed.
Data sharing is a key component of successful value-based models. By collaborating with payers and other providers to share and receive data, practices can understand how outcomes are achieved and impacted and then utilize that information to shape delivery of services.
Value-based models are a two-way street though and entail buy-in from insurers.
“It depends a lot on the payers in your market and whether they're willing to pursue those models in a way that supports independent practices,” Eagle said. “You have to be willing to do it as a practice but that's not enough. You have to have a payer that's willing to support the model as well too from their end.”
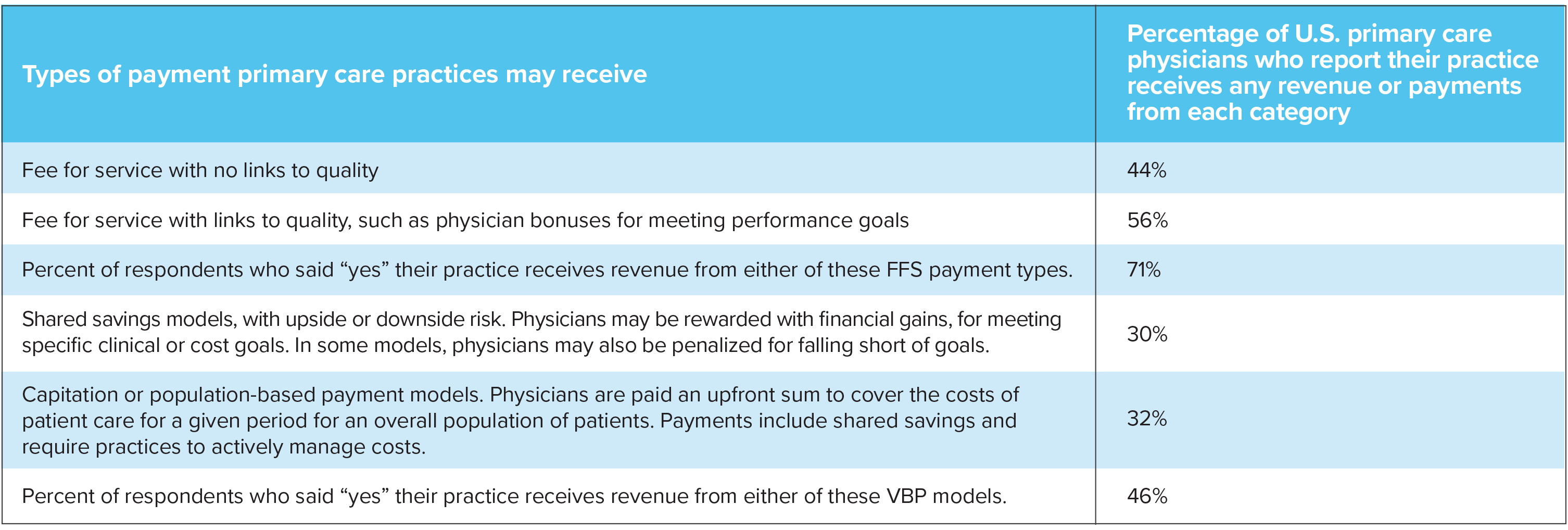
SOURCE: Celli Horstman and Corinne Lewis, “Engaging Primary Care in Value-Based Payment: New Findings from the 2022 Commonwealth Fund Survey of Primary Care Physicians,” To the Point (blog), Commonwealth Fund, Apr. 13, 2023. https://doi.org/10.26099/k3v8-0k69
Pursue Additional Revenue Streams
One way physicians must evolve, which was learned during the COVID-19 pandemic, is to embrace medicine that is both convenient and personalized.
Telehealth is a clear example of that. By offering that option to your patients, not only can it afford you the opportunity to slash expenses by downsizing office space, but it may also potentially bring in more patients that you otherwise wouldn’t see, thus increasing your revenue.
71%
percentage of surveyed physicians
that say they receive payment via a fee-for-service model.
“Telehealth in a lot of ways is sort of a triage,” Holder says. “It casts a wider net to make sure that the patients that need to see you in office are then coming to see you afterwards.”
By not offering some form of telehealth, you may be giving away the triage to someone else who has the power to recommend the next step of a patient’s care. Instead, you want to get that patient through your doors if telehealth isn’t enough to treat them.
On the flip side, practices can demonstrate their value as partners for bigger organizations who specialize in telehealth but don’t offer secondary, tertiary, or quaternary care. Those organizations need providers in individual markets who can provide those levels of service and by fostering relationships with them, your practice can be the next stop in their patients’ journey.
That can translate to growth for your practice, even if it’s not measured in the conventional sense like with the number of practice locations or number of patient visits in the office.
Percent of Office-Based Physicians That Used Telemedicine, 2018-2021
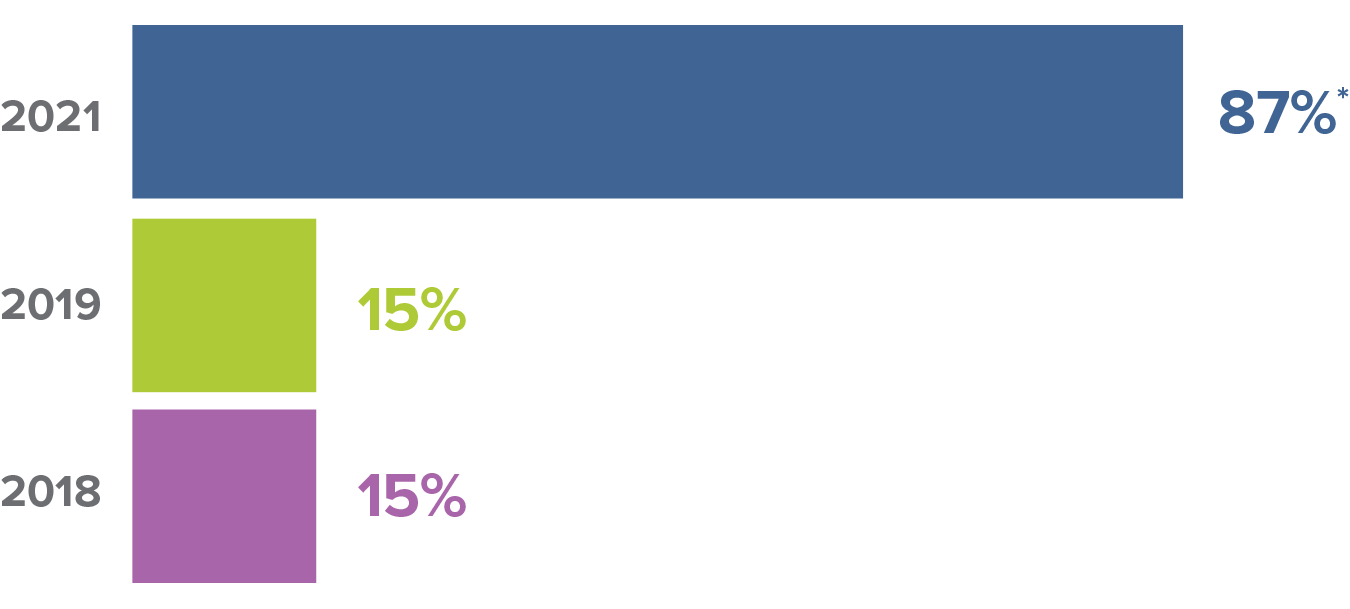
SOURCE: Source: National Electronic Health Record Survey, 2018-2021.
NOTES: Survey respondents are physicians who practice in office-based settings. See Definitions and a description of the data source and methods for more information. Significantly different from 2019, * p<0.05.
Utilizing technology in general needs to be a primary strategy for practices. That doesn’t necessarily mean you have to dive into the deep end with artificial intelligence. Investing in technology could include completely or partially owning something like an ambulatory surgery center or imaging center, which would be another source of revenue to buoy your practice so you are not reliant on just professional service fees.
“Traditional providers are going to have to figure out a way to mirror their cost structure to the services that they're providing instead of just using their existing cost structure because the reimbursement eventually won't stay the same for in-office versus out-of-office,” Holder says. “You have to be prepared to live in that world.”
Practices should also consider adding other specialties to widen your patient base and create more of a one-stop shop for care. You need to have the resources and relationships to bring other physicians under your umbrella, but it can greatly improve the financial health and sustainability of the practice. It won’t suddenly make you a direct competitor to hospitals, but it will inch you closer to their level in terms of the wide range of services provided.
An advantage independent practices do have over hospitals and health systems though is their agility. Whereas larger organizations move slower because of their scale and the amount of decision-makers involved, practices can be quicker to implement new ideas and understand their outcomes.
That is especially true in an ever-evolving area like technology, but it can also apply to most parts of the business. For example, practices can leverage the current workforce unrest in healthcare which is leading to labor strikes across the country by adjusting their pay scales for employees. It can make you an attractive employer and potentially cut down on turnover during a time when all providers are hoping to achieve that.
Ultimately, practices should constantly be thinking about ways to fulfill needs that are being unmet, whether it’s the needs of patients, payers, or anyone else that you are dependent on for survival.
“You have to realize that if there's if there's a demand for something in the marketplace and you’re not doing it, someone else is going to do it,” Holder says. “Someone will fill the gap.”
Jay Asser, Editor, HealthLeaders
