
COVER STORY
May 2025
Healthcare innovation is shifting from big, disruptive ideas to practical, problem-specific solutions. Is true transformation still possible in a system under relentless financial and operational pressure?


COVER STORY
May 2025
The Innovation Enigma: Can Healthcare Find (and Fund) the Right Path to Transformation?
Healthcare innovators are walking a fine line between big, disruptive ideas and practical, problem-specific solutions. Is true transformation still possible in a system under relentless financial and operational pressure?

TAKEAWAYS
-
Some of the biggest health systems in the country are showing vulnerability, highlighting the challenges that come with scooping up as much market share as possible.
-
An increase in size can negatively impact areas like quality and the workforce, putting further financial pressure on health systems.
-
Innovative partnerships and joint ventures, along with market realignment, offer opportunities for growth and optimization without the risks of excessive consolidation.
TAKEAWAYS
-
True healthcare innovation isn’t about moving faster—it’s about knowing when not to.
-
The best ideas in healthcare often start as quiet workarounds, not loud disruptions.
-
Chasing transformation without context turns innovation into just another operational expense.
Everyone talks about innovation like it’s an inevitable, shiny fix to healthcare’s most painful problems. But in today’s brutal financial climate, where margins are razor-thin and burnout runs high, is real innovation even possible? For all the talk of transformation, health systems are shackled by practicality.
C-Suite executives say innovation is imperative, but the journey from that lightbulb-over-the-head moment to broad clinical acceptance is tricky, and good ideas don’t necessarily work out just because they’re good.
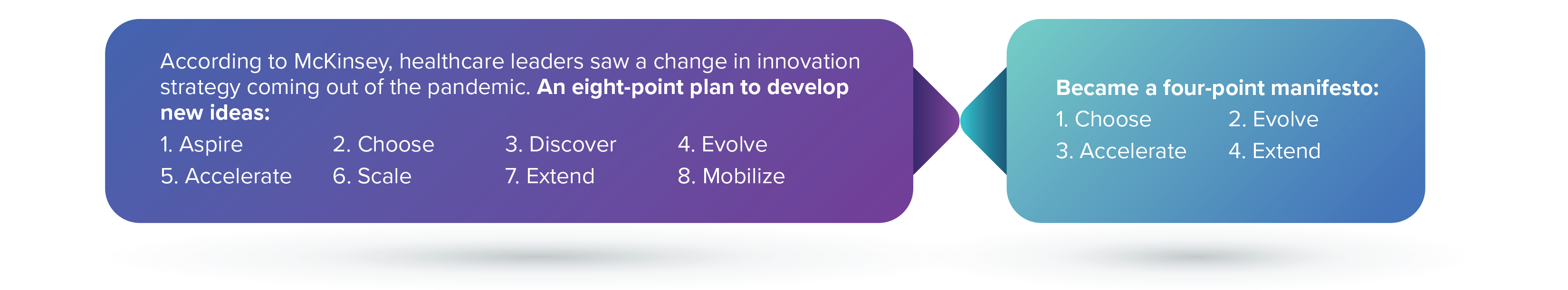
While many would have described the pace of healthcare innovation as slow and steady during the first two decades of this century, the COVID-19 pandemic threw everything in a blender and pressed puree.
Ideas that would normally take a few years to develop were put to the test in months, if not weeks. And while that era saw incredible growth, it also put the healthcare industry on notice, highlighting the shortcomings: Stress and burnout, leading to dwindling workforce numbers, unsustainable costs, and questionable value.
In other words, healthcare innovators have to speed up the pace but be deliberate and measured. They have to embrace new ideas but be selective. As Alannis Morissette might say, isn’t it ironic?
Finding That Balance
Steve Miff, president and CEO of the Parkland Center for Clinical Innovation (PCCI), a research center spun off from Parkland Health in 2012, says innovation is often broken off into two groups: Transformational technology and ideas that are often brought into the healthcare industry from outside disruptors or companies looking to make big changes; and smaller, targeted concepts usually introduced by clinicians or others within the health system who are targeted a specific pain point.
“More incremental innovation is [when] you see a line or a queue and say, ‘How do we make this go faster?” he says. “Transformative innovation is when we don’t have a queue to begin with.”
$3.3B
How much money AI-enabled digital health startups attracted in venture funding from January to October 2024.
Source: RockHealth
An example of the latter: During the height of the COVID-19 pandemic in 2021, nurses at The Ohio State University Wexner Medical Center struggled to manage blood glucose monitoring for diabetic patients in isolation. So, they created a digital health process by which to track patient levels and administer insulin without coming into direct contact with the patients.

Steve Miff
president and CEO of the Parkland Center for Clinical Innovation (PCCI)
An example of the former might be a virtual nursing platform that changes how healthcare is managed in the inpatient setting, or a Hospital at Home platform that extends acute care to patients at home. Those strategies target multiple pain points are require but-in from many different departments.
Both can have immense value to the health system or hospital, Miff says, but each has a different path to follow.
“The more transformative the innovation is, the less you actually really know the iterations that you're going to go through,” he says. That’s why it’s important to design a project in phases, with goals, metrics, a budget and defined ROI for each stage and the freedom to ditch the project or pivot at any stage if the results aren’t there.
“It’s really important to identify what success looks like and how and what you’re going to track,” Miff says. “A good innovation project has the flexibility to fail. Not everything is going to work.”
Healthcare executives need to develop a timeline for innovative projects, with an idea not only of how things might look in two, five, and 10 years but who would be impacted.
That’s something that health systems can easily overlook, with big ramifications. Miff says PCCI developed a trauma mortality module for the Emergency Department a while back (Parkland has one of the busiest Eds in the country).
“But a good innovation project has the flexibility to fail. Not everything is going to work.”
—Steve Miff, president and CEO of the Parkland Center for Clinical Innovation, a research center spun off from Parkland Health.
The technology was a hit with ED staff who were desperate for these tools, but the tool also impacted the ICU, inpatient care and others in the hospital, and they had different ideas and concerns.
In the case of AI, he says, many new algorithms are designed on a historical database, but they have to transition to a real-time database to be sustained and scaled. Too many health systems embrace a new AI tool, flip the switch and then can’t keep up with the demand for new data, leaving the new idea to flounder.
A new idea might also struggle just because the timing isn’t right. Miff says PCCI created a technology “genius bar” for patients several years ago. With funding from grants, the genius bar was deployed in a few clinics … and didn’t get much use. The problem was that people weren’t that interested in learning about new healthcare technology back then. PCCI took the project down and is relaunching it now, when the consumer technology market is much more popular and people are more interested in learning about technology.
“Failing early and often [is a good strategy],” says Miff, “but at the end of it you want it to solve a purpose. You want it to have an impact, you have to have a measurable outcome, and you want to deploy it.”
One Step Back, Two Steps Forward
Brenton Burns, EVP of UPMC Enterprises, says it’s sometimes difficult to get hospital executives to think beyond “here and now,” especially in light of the popular theory that innovation needs to show immediate ROI. Some truly transformative ideas, he says, require executives to “take that half a step back and then take two steps forward.”
UPMC Enterprises, the innovation, commercialization and venture capital arm of the Pittsburgh-based, 40+-hospital health system and health plan, was launched in 2014 “to be in front of the best ideas in healthcare,” says Burns, who joined the organization soon after its launch. He estimates he sees more than 500 new opportunities a year.

Brenton Burns
EVP of UPMC Enterprises
“[Healthcare innovators] are incredible firefighters. What we’re not always the best at is fire prevention.”
—Brent Burns, EVP of UPMC Enterprises.
The organization’s strategy is familiar. Burns says they scout the landscape for startups and small companies that have interesting ideas and need s little push, either through support or a partnership.
“Most the time we will find the makings of a solid start of a solution that we can help evolve over time to really meet our needs of our clinicians and patients,” he says.
Burns says healthcare innovation has a fundamental problem that’s plaguing the entire industry, and which forms the foundation for the value-based care movement.
“We are incredible firefighters,” he says. “What we’re not always the best at is fire prevention.”
He has a valid point.
Many new ideas and technologies in healthcare were created to answer problems and address obvious and glaring pain points. Even AI, held up as having the potential to transform the entire industry, is being embraced because, quite honestly, healthcare has to change. There is so much wrong in the industry these days that health systems and hospitals risk total collapse if they don’t become innovative.
So, with their backs against the wall, healthcare executives are gung-ho for innovation. But they should also be looking farther ahead and identifying opportunities for transformation that aren’t based on today’s deficits. Like the idea that healthcare should focus more on health and wellness and prevention, healthcare innovation should prepare the industry for the future, rather than just making sure the doors stay open this year.
What is hindering technology innovation?

SOURCE: Technology Innovation in Healthcare Survey, HIMSS Media
Playing the Long Game
Becky Buchen, senior vice president of innovation operations at OSF HealthCare, says healthcare innovation is a long and careful process, requiring plenty of checks and balances.
“Innovation without the rigor is just going to lead to chaos,” she points out. “That’s not necessarily transformational.”
“Innovation without the rigor is just going to lead to chaos. That’s not necessarily transfor-mational.”
—Becky Buchen, senior vice president of innovation operations at OSF HealthCare.
The first step to analyzing a new idea or technology, she says, is to understand what pain point it expects to address.
“We're really saying, OK, what's the problem?” she says. “We don't bring in a solution looking for a problem. We're bringing the problem forward first and … scanning the landscape to understand, is there a solution out there that we could try and see if it works? It is a process.”

Becky Buchen
senior vice president of innovation operations at OSF HealthCare
“Sometimes we just say, ‘Let's sit down and talk about your day,’” she says. “And when you hear about the concerns you also hear [about] all the workarounds. This is how we deal with it. Then you say, ‘OK, like maybe there's a different way.’”
In these conversations, she says, innovation leaders learn a lot about the people they’re helping—not only the patients whose health concerns are being addressed, but the nurses and doctors who shape care delivery. A brand-new AI tool or virtual care platform might be really transformative, but it will only work if the people using that technology are willing to make that leap.
“Innovation is certainly always about the outcomes,” she says, “but it's as much about the learnings as it is about the technology itself.”
Eric Wicklund is the associate content manager and senior editor for Innovation at HealthLeaders