
COVER STORY
November 2025
Eliminating Workplace Violence Is Impossible. Here’s How Health System Leaders Are Fighting Back.
As violence against healthcare workers surges—from verbal assaults to physical attacks—hospitals are confronting a grim reality, prevention isn’t enough. Leaders must respond with urgency, compassion, and courage to protect their people, heal their teams, and hold perpetrators accountable.


COVER STORY
November 2025
Eliminating Workplace Violence Is Impossible. Here’s How Health System Leaders Are Fighting Back.
As violence against healthcare workers surges—from verbal assaults to physical attacks—hospitals are confronting a grim reality, prevention isn’t enough. Leaders must respond with urgency, compassion, and courage to protect their people, heal their teams, and hold perpetrators accountable.

TAKEAWAYS
- ith • After a violent incident, healthcare organizations can’t wait for staff to seek help. Leaders must reach out immediately to ensure physical safety, emotional recovery, and long-term resilience.
-
When patients cross the line, care has limits. In cases of severe aggression or abuse, hospitals must be prepared to take decisive action, including administratively discharging violent patients to protect their teams.
- Helping staff members press charges and navigate the legal process reinforces accountability and shows that violence against caregivers will not be tolerated.
TAKEAWAYS
- After a violent incident, healthcare organizations can’t wait for staff to seek help. Leaders must reach out immediately to ensure physical safety, emotional recovery, and long-term resilience.
-
When patients cross the line, care has limits. In cases of severe aggression or abuse, hospitals must be prepared to take decisive action, including administratively discharging violent patients to protect their teams.
- Helping staff members press charges and navigate the legal process reinforces accountability and shows that violence against caregivers will not be tolerated.
The frontlines of healthcare have become battlegrounds. From emergency departments to outpatient clinics, nurses, physicians, and staff are increasingly finding themselves under attack—verbally, emotionally, and physically—by the very people they’re trying to help.
Despite years of investment in training, security, and prevention, the crisis of workplace violence continues to escalate, leaving caregivers traumatized and organizations reeling.
Now, health systems across the country are taking a harder line. They’re adopting aggressive response protocols, empowering staff to press charges, and even discharging violent patients. They’re pairing psychological support with legal advocacy and transforming lessons from every incident into systemwide action.
Their message is clear: while eliminating workplace violence may be impossible, quietly moving on is no longer an option.
How did we get here and where do we go?
Violence in healthcare is not new, but it’s only continuing to escalate.
A study of outpatient physician clinics found that as many as 59.3% of physicians, 62.1% of nurses, 68.4% of receptionists, and 40.0% of technicians had experienced workplace violence. In 2023, the financial cost of workplace violence for hospitals was estimated at $18.27 billion, according to a study conducted by the American Hospital Association.
When workplace violence occurs, healthcare organizations must respond swiftly and comprehensively.
“First and foremost, we make sure staff are physically safe after an event,” says Ghazala Sharieff, MD, MBA, corporate executive senior vice president as well as chief medical and operations officer of acute care at Scripps Health.
“If there are any injuries, we send staff members to the emergency department. Then there is the mental health component. Sometimes, staff members may seem strong after a workplace violence incident, but in the hours after an incident and after a staff member goes home after their shift, I am concerned about their mental health.”
Scripps Health does not wait for affected staff members to reach out for help. When a workplace violence incident occurs, the health system’s employee assistance program and Resilience in Stressful Events (RISE) program contact affected staff members.
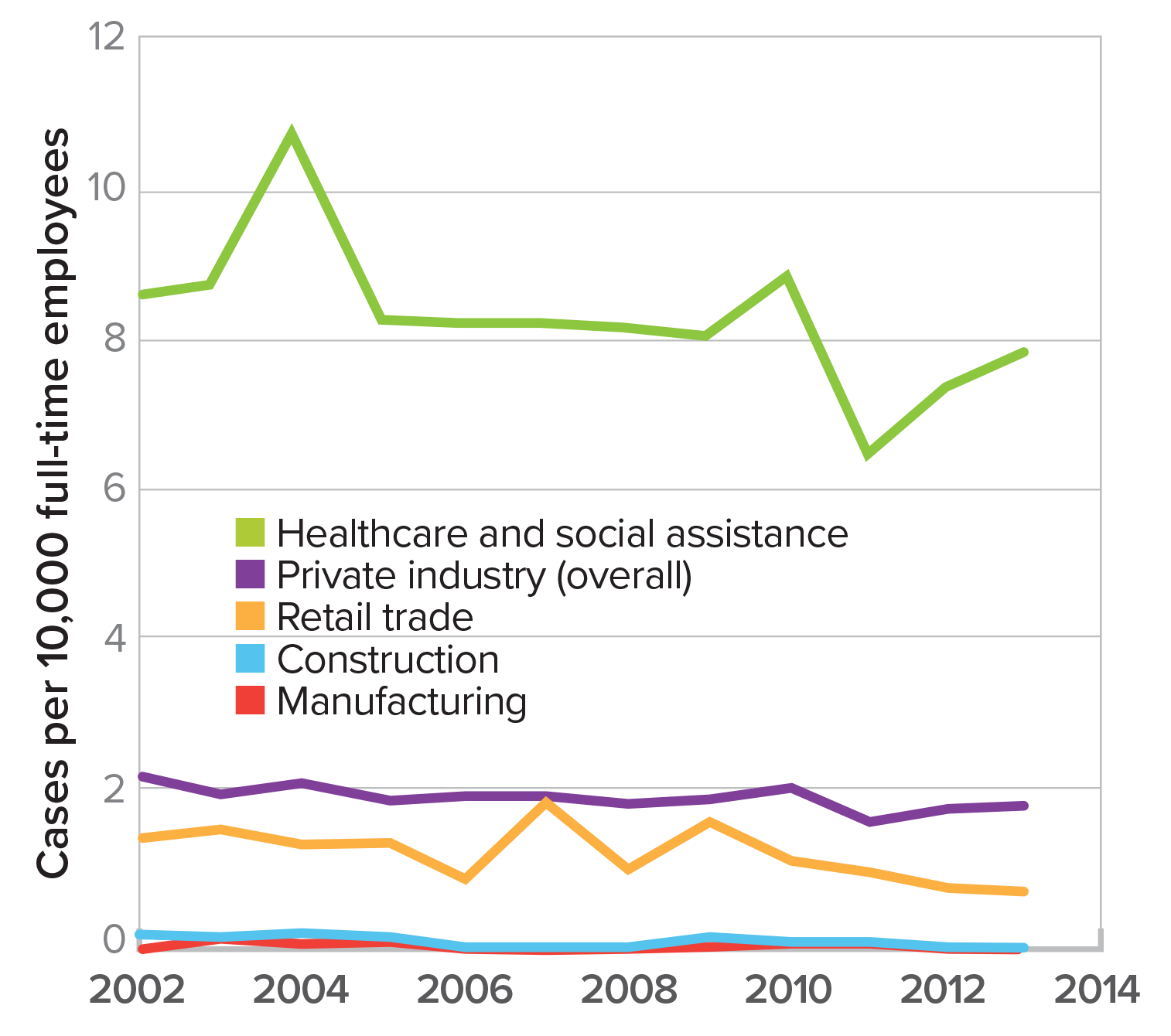
SOURCE: OSHA/Labor of Statistics
59%
of physicians and 62% of nurses have experienced workplace violence in outpatient clinics.
Source: NIH
“Physicians in particular are reluctant to reach out for help from psychologists and other professionals, so the RISE program provides physician peer-to-peer responders to reach out directly to physicians involved in workplace violence incidents to give them support and someone to talk to,“ Sharieff says.
The process of reaching out to staff members after a workplace violence incident should include a prompt investigation of the event.
“As soon as possible, we hold a debriefing that is blame free for staff members and focuses on listening to staff members about information that we can subsequently use to make the environment safer and to protect our workforce,” says Carolyn Kloek, MD, MBA, CMO at OU Health.
At OU Health, the workplace violence debriefing process includes gathering any staff members involved in an incident as well as key leaders.
“We try to get as much information as possible about what happened, so we can understand what happened to learn from it and prevent similar incidents from happening in the future,” Kloek says. “We want to learn from incidents to mitigate safety risks. Everybody has different perspectives, and we want to get the full diversity of perspectives on the situation when it is still fresh in people’s minds.”
To analyze workplace violence incidents, Scripps Health applies the F3EAD methodology, which stands for Find, Fix, Finish, Exploit, Analyze, and Disseminate.
“It’s a way to systematically address high-risk environments,” says Todd Walbridge, senior director of safety and security at the health system.
Find involves identifying the risks, the hot spots, and repeat offenders. Fix involves whether there is a technology fix, educational fix, or training fix. Finish involves determining whether the fix that was applied provided an effective solution. Exploit and analyze involves looking at the data to see whether what was found and fixed created a change in the propensity of workplace violence incidents. Finally, the health system disseminates information gained through the F3EAD process across the enterprise, so that every lesson is passed on.

Ghazala Sharieff, MD, MBA
corporate executive senior vice president, chief medical and operations officer of acute care, Scripps Health
Healthcare organization leaders should follow up with staff members who are affected by workplace violence incidents in the weeks and months following an event.
”It is important to recognize that this is often not a ‘one and done’ situation,” says Juliann Barrett, DO, MBA, CMO of Valley Regional Hospital, which is part of Dartmouth Health. “The emotional sequela of these events might not manifest for days or even weeks after the incident, so even employees who said they were ‘OK’ immediately after an event need longitudinal check-ins.”
Scripps Health uses the F3EAD methodology—Find, Fix, Finish, Exploit, Analyze, and Disseminate—to analyze workplace violence incidents.
“It’s a way to systematically address high-risk environments,” says Todd Walbridge, senior director of safety and security at Scripps Health.
- Find: Identify risks, hot spots, and repeat offenders.
- Fix: Determine whether a technology, education, or training intervention is needed.
- Finish: Evaluate whether the solution worked.
- Exploit & Analyze: Examine data to determine whether interventions reduced incidents.
- Disseminate: Share lessons learned across the organization.
Administrative discharge
For severe workplace violence incidents involving patients as perpetrators, health systems and hospitals can administratively discharge patients.
“If patients in the hospital setting need to be discharged because of severe violent behaviors, that gets escalated up to the executive level, and we review all the information to make the decision on whether we are going to administratively discharge a patient,” says Natalie Nicholson, DNP, MBA, CNO of Denver Health and executive sponsor of the health system's Workplace Safety Violence Prevention Committee.
Denver Health employs several interventions before the administrative discharge of a patient.
“The care team reviews the care plan, and they determine whether the patient needs a change in medication and whether the patient is stable medically,” Nicholson says. “The nurse manager or another leader will have a conversation with the patient. The attending physician will have a conversation with the patient. Security staff will have a conversation with the patient. So, there are multiple touchpoints to get the patient to choose better behaviors.”
Examples of behavior that can result in a Denver Health patient being administratively discharged include sexually inappropriate behavior such as grabbing a nurse or making advances as well as violent behavior such as choking and punching, according to Sarah Gardiner, MSN, RN, associate CNO at the health system and co-chair of the Workplace Safety Violence Prevention Committee.
For an administrative discharge to move forward, a Denver Health patient must be capable of understanding that their behavior is unacceptable.

Carolyn Kloek, MD, MBA
CMO,
OU Health

Todd Walbridge
senior director of safety and security,
Scripps Health
“Getting justice is often part of healing. Filing charges and prosecuting perpetrators shows our employees that their safety truly matters.”
—Todd Walbridge, Senior Director of Safety and Security, Scripps Health
“For an administrative discharge, the patient must be aware of their behavior,” Gardiner says. “There are many diagnoses where the patient is not coherent or aware of their behavior.”
It is easier to conduct an administrative discharge of a patient in the ambulatory setting, and the process cannot be applied in emergency departments, according to Sharieff.
“The process involved in administratively discharging patients includes meeting with the patient, engaging our legal team, and crafting an official letter,” Sharieff says.
Acts of violence or repeated instances of verbal abuse can result in a patient being administratively discharged at Scripps Health.
“If you can’t de-escalate a situation, and if you have tried everything including involving supervisors to address a patient’s bad behavior, but there is a pattern of physical or verbal abuse, then we go through our process to administratively discharge a patient,” Sharieff says.

Juliann Barrett, DO, MBA
CMO,
Valley Regional Hospital

Natalie Nicholson, DNP, MBA
CNO,
Denver Health
Filing charges
After a workplace violence incident occurs, encouraging staff members to file charges can help them get past the event.
“In workplace violence incidents, getting justice for what happened to you is an important part of the healing process,” Walbridge says. “This includes filing charges, working with law enforcement, and prosecuting perpetrators.”
Particularly for several workplace violence incidents, Denver Health encourages employees to file charges, according to Nicholson.
“If they file charges with the police, then we have our security team provide support in filing that report,” Nicholson says. “There are victims’ advocates from the district attorney’s office that are assigned to the staff member who was assaulted, and they help the staff member through the process after charges have been filed and going to court."
Frontline leaders such as nurse managers will also work with the employee to make sure that they can have time off to go to court, Nicholson adds.
To help staff members through the process of filing charges, Scripps Health also works with the local district attorney’s office and has created an intranet site called Workplace Violence: Your Rights and Protections.
“For example, a victim may want to know if they file a complaint will it go to trial, will they have to testify, or will they have to face the perpetrator,” Walbridge says. “The district attorney’s office put together a frequently asked questions document that we have posted on our intranet site and links to the district attorney's website.”
Walbridge, who is a former FBI agent, gets involved when staff members file charges.
“If a workplace violence incident ends up in court, I will go to court with the employee and sit with them in court,” Walbridge says. “As a veteran of law enforcement, I have testified many times, so I can help the employee through the anxiety of testifying.”
“If patients become violent, we review every detail—and when necessary, we make the hard call to administratively discharge them. Protecting our staff comes first.”
—Natalie Nicholson, DNP, MBA, Chief Nursing Officer, Denver Health

Sarah Gardiner, MSN, RN
associate CNO, and co-chair of the Workplace Safety Violence Prevention Committee, Denver Health

Scott Strauss
vice president of corporate security, Northwell Health
Learning from workplace violence incidents
As part of the learning process after a workplace violence incident, leaders should ensure that their organization was properly prepared to respond, according to Scott Strauss, vice president of corporate security at Northwell Health.
“Executives should have their policies and/or procedures reviewed and determine whether adjustments or additional training and education are needed,” Strauss says.
Learning from workplace violence is not just about examining single incidents, Walbridge explains.
“It involves how we handle all of our incidents as an enterprise and collectively try to apply lessons learned to make everything better for the next employee who experiences workplace violence,” Walbridge says.
Disseminating what is learned from workplace violence incidents is crucial, according to Sharieff.
“If an incident occurs at one site, we want to bring the learnings from that incident to other sites and how we can prevent the incident from occurring at another site,” Sharieff says. “You do not want to let an incident slide and wait for another incident to happen.”
Part of the learning process is looking for patterns, Kloek explains.
“Sometimes, these incidents can seem isolated, but when you look at incidents over time, you can see trends,” Kloek says. “For example, certain areas can have higher rates of workplace violence incidents, and the pattern recognition can help us direct where to focus prevention efforts for the future.”
Members of the leadership team need to be present and engaged to promote learning from workplace violence incidents, according to Barrett.
“When a workplace violence event occurs, frontline staff need to see executive leadership,” Barrett says. “They need to receive direct support from their executive leaders. They need to voice their concerns and experiences directly to the highest levels of leadership. They need to be encouraged to open up and talk. When a workplace violence event takes place, presence is one of the most valuable tools to comfort, support, learn, and heal.”
Christopher Cheney, CMO Editor, HealthLeaders
Subscribe to HealthLeaders CMO Newsletter + Daily Briefing
By subscribing to HealthLeaders I agree to sign up to receive newsletters and special offers. I understand that I can opt out at any time. Privacy policy.