
COVER STORY
July 2025
During a time of extreme scrutiny, nursing’s commitment to diversity and health equity remains, but how do healthcare leaders preserve the spirit of diversity when the very terminology has been weaponized?


COVER STORY
July 2025
Diversity, Equity and Inclusion in Nursing Must Endure. Here’s How to Preserve It.
During a time of extreme scrutiny, nursing’s commitment to diversity and health equity remains, but how do healthcare leaders preserve the spirit of diversity when the very terminology has been weaponized?

TAKEAWAYS
- Not only is DEI integral to the nursing code of ethics, having a diverse workforce improves patient outcomes.
-
CNOs should examine their DEI programs and policies that currently exist, and work to balance compliance with legal and regulatory requirements with professional and ethical standards and obligations.
- CNOs and other healthcare executives should consider taking steps to revisit their approaches, programs and policies while maintaining the nursing code of ethics.
TAKEAWAYS
- Not only is DEI integral to the nursing code of ethics, having a diverse workforce improves patient outcomes.
-
CNOs should examine their DEI programs and policies that currently exist, and work to balance compliance with legal and regulatory requirements with professional and ethical standards and obligations.
-
CNOs and other healthcare executives should consider taking steps to revisit their approaches, programs and policies while maintaining the nursing code of ethics.
Diversity, equity, and inclusion (DEI). Seems like a no-brainer in nursing, right?
Since the beginning of the year, stark criticism and negative connotations of the concept of DEI has swept throughout the country, pushed largely by the Trump Administration and their constituents.
On January 20, an executive order (EO 14151) titled "Ending Radical And Wasteful Government DEI Programs And Preferencing" began the termination of diversity, equity, inclusion, and accessibility (DEIA) initiatives across all federal agencies and their contractors.
The language is stark: end the programs, rescind the funding, erase the mandates—no matter what name they go by.
The EO directed the withdrawal of federal funding from all federal contractors who have provided DEI training or materials to employees as well as any federal grantees who have received funding to provide or advance DEI, DEIA, or environmental justice programs since January 21, 2021.
A second EO, titled "Ending Illegal Discrimination and Restoring Merit-Based Opportunity" (EO 14173), ordered the termination of all discriminatory and illegal preferences, mandates, policies, programs, activities, guidance, regulations, enforcement actions, consent orders, and requirements. This EO also calls for the enforcement of "longstanding civil-rights laws" and the combating of "illegal private-sector DEI preferences, mandates, policies, programs, and activities."
Together, these orders have sparked chaos across hospitals and health systems, many of which rely on federal funds to support community-based DEI initiatives, training, and leadership pathways. Now, pending legal challenges to the EOs and some key provisions, legal teams scramble to determine the line between compliance and conscience.
But here’s the truth no one can scrub from a statute: nurses still show up every day to care for patients from every walk of life. They see the disparities. They feel the gaps. They know that representation, cultural humility, and inclusive environments aren’t political—they’re essential.
So, if the playbook has been stripped away, what’s next? How do nurse leaders preserve the spirit of diversity when the very terminology has been weaponized?
The future of equitable care hangs in the balance—and some CNOs are stepping up to lead through the uncertainty.
Diversity is the directive
First off, it's important for CNOs to refocus on why diversity is critical in the nursing profession. According to Katie Boston-Leary, senior vice president of equity and engagement at the American Nurses Association (ANA), and HealthLeaders Exchange member, this issue sits at the core of nursing as a profession.
"The key thing I think a number of nurses are taking away is the fact that this work is not debatable, because part of our core and what makes us, us, is our code of ethics that ANA recently released," Boston-Leary said, “and it goes into really good detail around how equity work is about who we are and it's what we do every day."
To Boston-Leary, the biggest thing to remember is to not get caught up on verbiage, and to focus on nursing practice.
"So long as we focus on the work to make sure that we are not causing harm and we're leveling the playing field in terms of outcomes for all people that rely on us for their care, that's essentially what it is," Boston-Leary said.
The nursing workforce in the United States is also not as diverse as it should be, according to Boston-Leary.
"The reason that is important is because once we diversify the nursing workforce, that will help us improve outcomes for all people," Boston-Leary said. "That is our charge, that is our directive, and we must keep going regardless."
Growing Share of U.S. Workers Say Focusing On DEI At Work Is A Bad Thing

SOURCE: Per Research Center
To Stephan Davis, executive director of leadership, policy, and DNP education, and associate professor, doctor of nursing practice programs and the Georgetown University School of Nursing, there is a broad consensus among healthcare leaders that supports the bioethical principles of autonomy, beneficence, nonmaleficence and justice. Davis describes advancing inclusion as a moral imperative.
"Discrimination or harm based on identity is fundamentally incompatible with ethical practices," Davis said. "Upholding our work to advance diversity and inclusion, at its core, is an expression of our ethical commitment to respect, serve, protect, and fairly treat every individual and all communities."

Katie Boston-Leary
senior vice president of equity and engagement at the American Nurses Association (ANA)
In addition to the legal standing of DEI programs in the U.S., attitudes among American workforces are also looking grim. According to a 2024 data from the Pew Research Center, 52% of working adults believe that focusing on DEI principles at work is a good thing. That number fell from 56% in 2023. In that same period of time, the number of workers who believe focusing on DEI at work is a bad thing rose from 16% to 21%.
Davis explained that these shifts are occurring alongside broader political and legal changes, including the 2023 Supreme Court decision to eliminate affirmative action in college admissions and the increasing efforts to ban or restrict DEI initiatives.
"Healthcare and nursing are not immune to these sociopolitical shifts," Davis said. "In some cases, we have seen prominent organizations eliminate executive roles focused on DEI, and professional associations remove public-facing materials that once centered diversity and inclusion."
According to the Bureau of Labor Statistics (BLS), as of 2024, 86.6% of registered nurses (RN) are women and 72% are white. Only 15.8% of RNs are black of African American, 9.8% are Asian, and 9.8% are Hispanic or Latino.
For nurse practitioners, 88.1% are women, 78.1% are white, 11.7% are black or African American, 9.5% are Asian, and 6.8% are Hispanic or Latino. For LPNs and LVNs, 89.6% are women, 58.3% are white, 30.4% are black or African American, 7.2% are Asian, and 15.9% are Hispanic or Latino.
As with other professions, the distribution of these nurses largely depends on geographical location, and the U.S. becomes a progressively more diverse country, it's critical that the nursing profession keeps up. According to a 2019 umbrella review, studies have shown that patients have better outcomes under more diverse care teams, and organizations see better financial results.
However, DEI is not just about racial diversity, according to Boston-Leary. Other aspects of diversity include gender identity and expression, socioeconomic status, disability status, and neurodivergence, along with faith and religious traditions, sexual orientation, veteran status, and more.
"It's about all aspects of diversity, everything that makes us unique, everything that makes us different, even though I continue to stress as well that there's more that unites us than divides us," Boston-Leary said.
“It’s about all aspects of diversity, everything that makes us unique, everything that makes us different, even though I continue to stress as well that there’s more that unites us than divides us.”
—Katie Boston-Leary, senior vice president of equity and engagement at the American Nurses Association.
Boston-Leary emphasized that welcoming everyone into the nursing profession is the only way to provide the best care that patients deserve.
"We should no longer be splintering who's who and who's where, who belongs in the profession, and who doesn't," Boston-Leary said. "This profession is for everyone, regardless of their background, their socioeconomic status, how they present in terms of any disabilities that we have, seen or unseen."
Integrating core values
The next step for CNOs is to build a robust, nursing-focused equity-minded program that benefits the nurse, the patient, and the organization. According to Boston-Leary, examining the systems and structures that currently exist within organizations is a great place to start.
"I think it really boils down to taking a hard look at our policies [and] the structures that are in place that uphold a lot if what's wrong with the way things operate today, and addressing them accordingly so that there is equity in a lot of the things that we do," Boston-Leary said.
Boston-Leary emphasized that a lot of these issues go unnoticed, and if left unaddressed for too long, they become normalized. CNOs need to take several looks at their policies to make sure that they aren't perpetuating and replicating harm.
"Then it takes leaders engaging in some level of humility and having some openness and adaptability, and also being collaborative to make sure that they're understanding all viewpoints when it comes to this work," Boston-Leary said.
Davis emphasized that inclusive leadership is essential, and that CNOs must work to intentionally cultivate work environments where nurses from every background feel valued, supported, and empowered to thrive.

Stephan Davis
executive director of leadership, policy, and DNP education, and associate professor, doctor of nursing practice programs and the Georgetown University School of Nursing
"One critical benchmark for this effort is ensuring that the nursing workforce, including leadership and governance structures, reflects the diversity of the communities served," Davis said. "As diversity within teams increases, so does the potential for innovation, empathy, and culturally informed practice."
The ANA recommends steps to promote diversity in healthcare organizations and nursing practice. Nurse leaders need inclusive recruitment, hiring, and retention strategies to build a strong, diverse team. Reevaluate recruiting processes to eliminate potential biases and advertise through various platforms using inclusive language. Organizations should develop and implement protocols that protect nurses from discrimination and violence and hold all individuals accountable for their behavior.
The ANA emphasizes the importance of building cultural humility with educational resources, which can help nurses learn how to best meet their patients' social, linguistic, and cultural needs. This training should be evaluated and edited to eliminate harmful stereotypes.
“CNOs must also institutionalize inclusive leadership by promoting equitable advancement opportunities, shared governance models, and policies and practices that honor the full range of lived experiences.”
—Stephan Davis, executive director of leadership, policy, and DNP education, and associate professor, doctor of nursing practice programs and the Georgetown University School of Nursing.
The second step is to reevaluate recruiting processes to eliminate potential biases and advertise through various platforms using inclusive language.
Third, organizations should partner with organizations in their communities, such as schools and universities, to help foster diversity in nursing education. The ANA recommends that nurse leaders look to established organizations for more resources and consider establishing an internal diversity committee.
Lastly, CNOs and other nurse leaders must lead by example and manage their bias and set a tone of inclusivity. CNOs should facilitate open conversations about complex topics and be willing to receive others' perspectives and feedback with empathy and respect.
To Davis, diversity alone is not enough.
"CNOs must also institutionalize inclusive leadership by promoting equitable advancement opportunities, shared governance models, and policies and practices that honor the full range of lived experiences," Davis said.
Integrating DEI efforts into strategies and policies also must include accountability metrics, Davis explained.
"CNOs should ensure that key performance indicators include equity-focused measures, such as disaggregated patient outcomes, workforce retention and advancement data by demographic, and progress toward eliminating health disparities," Davis said.
Age Distribution of RNs, 2015–2024
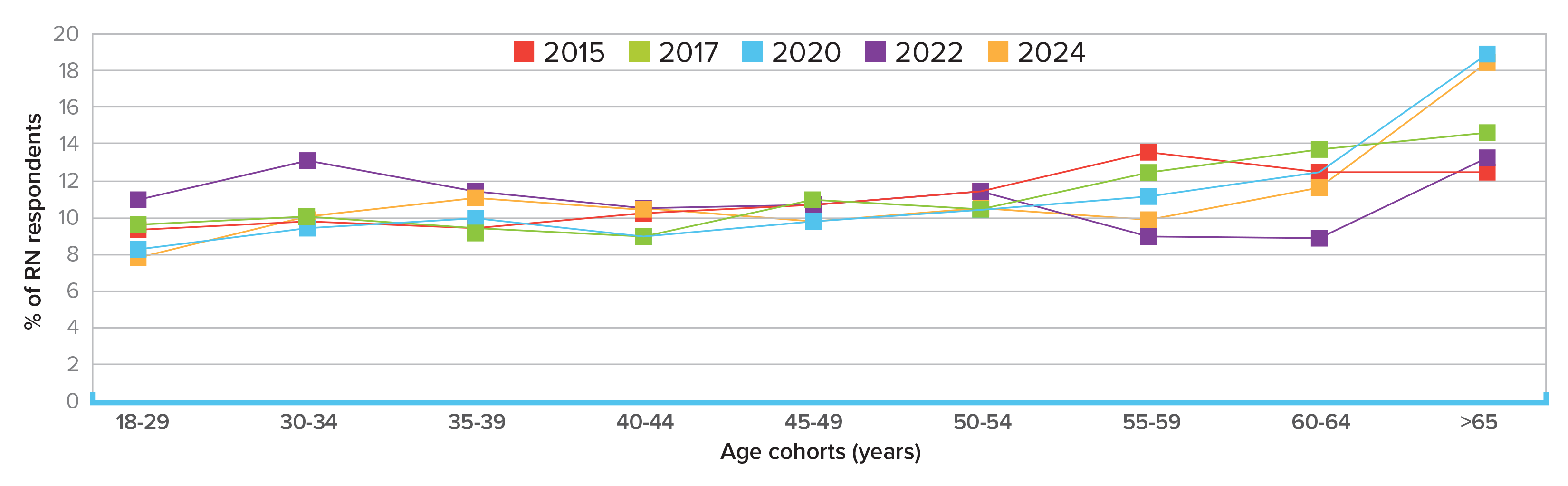
NOTE: RN = registrered nurse SOURCE: Journal of Nursing Regulations
Securing the future of nursing
While there is so much scrutiny surrounding DEI in every industry, CNOs and other healthcare executives might consider taking steps to reevaluate their programs and policies based on their risk tolerance and organizational values. The goal is to balance the core values of programs while also protecting organizations from outside scrutiny and backlash. As the ANA also takes these steps, Boston-Leary explained that it's all about risk.
"We want to understand political risk, reputational risk, financial risk, all various levels of risk, right?" Boston-Leary said. "It's important for us, in every instance, on an individual level and the system level, you have to understand your risk tolerance and adjust accordingly (or not)."
“This work, for us to make sure that we’re being equitable in care delivery, is part of who we are, and if there's any question about it, the most recently released code of ethics makes it very clear.”
—Katie Boston-Leary
Health system leaders should assess risk versus reward, and any steps they would take to mitigate that risk. Boston-Leary emphasized that it's important for CNOs and other leaders to stay as informed and adept as possible.
"Really take the time to read the executive order, understand how and whether it applies to your organization," Boston-Leary said. "Make that determination in terms of how it may impact you and your organization, [and] if you need to make some changes to language."
While language isn't the end all be all, it does matter, according to Boston-Leary.
"Every institution should take the time and understand what words should describe the current state and illustrate the future state to improve care delivery to the marginalized and minoritized," Boston-Leary said. “Words do matter.”
Davis recommends rebranding using phrases like "inclusive excellence," "belonging and well-being," or "human flourishing" to broaden the understanding of programs and to invite engagement from those across ideological lines. Shifting language and phrasing can help avoid misinterpretation and clarify DEI and the goals of diversity practitioners.
"In an organization truly committed to inclusive excellence, this work focuses on creating environments where everyone is included—and is not singularly focused on those from backgrounds that have been historically or systematically excluded," Davis said.
Nursing Labor Force Statistics from the Current Population Survey

SOURCE: U.S. Bureau of Labor Statistics
Davis emphasized that the tendency of some diversity leaders to narrowly focus on race and gender has contributed to the misconception that DEI is not for everyone. DEI leaders must focus on the full range of human experiences.
"Leaders must engage with diverse members across their organizations, including those who may be skeptical of formal DEI efforts, to determine the most effective path forward," Davis said. "The ultimate goal remains the same: ensuring that everyone has a fair chance to reach their full potential."
Ultimately, promoting diversity comes down to fulfilling the obligation that nurses have to patients.
"This work, for us to make sure that we're being equitable in care delivery, is part of who we are, and if there's any question about it, the most recently released code of ethics makes it very clear," Boston-Leary said.
It's critical for CNOs to continue fostering a psychologically safe environment for nurses during this time by being transparent and vulnerable with teams. Boston-Leary explained that while many leaders are culturally taught not to show how they are feeling, nurses respond better to vulnerability and authenticity. If nurse leaders sound inauthentic, nurses will start to feel afraid and distance themselves from those they feel are not interested in or don't believe in their work.
“In these moments, we must lean on our values and ethical principles to guide our decisions. They anchor us in what matters most—and ensure that our actions remain aligned with our purpose and professional obligations and commitments.”
—Stephan Davis
"They deserve to understand us, who we are as people, what's important to us, what our values are, and what we ascribe to, in addition to the organization that you work for," Boston-Leary said. "Otherwise, you're going to sound like company speak, and you don't want to sound inauthentic."
Davis emphasized that CNOs must go beyond creating safe spaces and intentionally build community and foster connection to achieve the safety and security that allows nurses to thrive.
"True psychological safety exists when team members are not only encouraged to voice concerns, but when dissent is welcomed and rewarded, especially when offering a contrary perspective leads to improvement," Davis said. "This is how nursing leaders can model inclusive leadership and promote psychologically safe environments where all voices are heard and valued."
For CNOs who are trying to continue their DEI initiatives despite the scrutiny, Boston-Leary recommends staying the course and to know that this is not the time to stay isolated, it's the time to build coalitions and set up win-win solutions.
"We have to make sure that we're more outcomes-focused and less performative," Boston-Leary said. "This is the right side of history time for folks in terms of where you're going to be, and when this is written about years from now, you want people to understand fully where you were and what you did as a leader."
While there might not be a straightforward "right" answer that satisfies all stakeholders, Davis recommends staying as focused as possible on mission, values, and the foundational principles of bioethics.
"In these moments, we must lean on our values and ethical principles to guide our decisions," Davis said. "They anchor us in what matters most—and ensure that our actions remain aligned with our purpose and professional obligations and commitments."
Editor’s note: The views expressed by Stephan Davis are his own and do not necessarily reflect the positions of any organizations he is affiliated with.
G Hatfield, CNO Editor, HealthLeaders